“This procedure/medication will require prior-authorization.” Words that no patient wants to hear when they are ready to proceed with a doctor-approved treatment plan for their medical concerns. However, it is one of the utilization management tools that insurance companies have developed to determine whether certain prescribed procedures, services, and medications are medically necessary, or whether there is an equally effective treatment available to the patient.
More often than not, when a physician decides on a course of treatment for the patient that would require prior-authorization (also referred to as pre-authorization), the doctor will inform the patient and their office will manage the process of putting in the request for approval to the insurance company. However, to be on the safe side, it is in the patient’s best interests to contact the insurance company themselves.
Blue Cross and Blue Shield of Michigan list the following as the types of treatment that typically need approval are those that:
- Can be considered cosmetic (example: Botox for migraine headaches)
- Have a lower-cost, equally effective alternatives (such as an available generic medication)
- Could be dangerous in and of itself
- Could be dangerous when combined with other drugs
- Can be misused or abused (example: Adderall)
- Are only necessary for certain types of medical conditions
The list of treatments requiring pre-authorization will vary by insurance company, so if you are changing insurance carriers, it is important to find out what they will/will not cover. Not only will the rules vary by insurance carrier, but the requirements for obtaining pre-authorization can also vary by the specific procedure/medication requiring approval.
For example, the use of Botox for migraine headaches, may require, among other things:
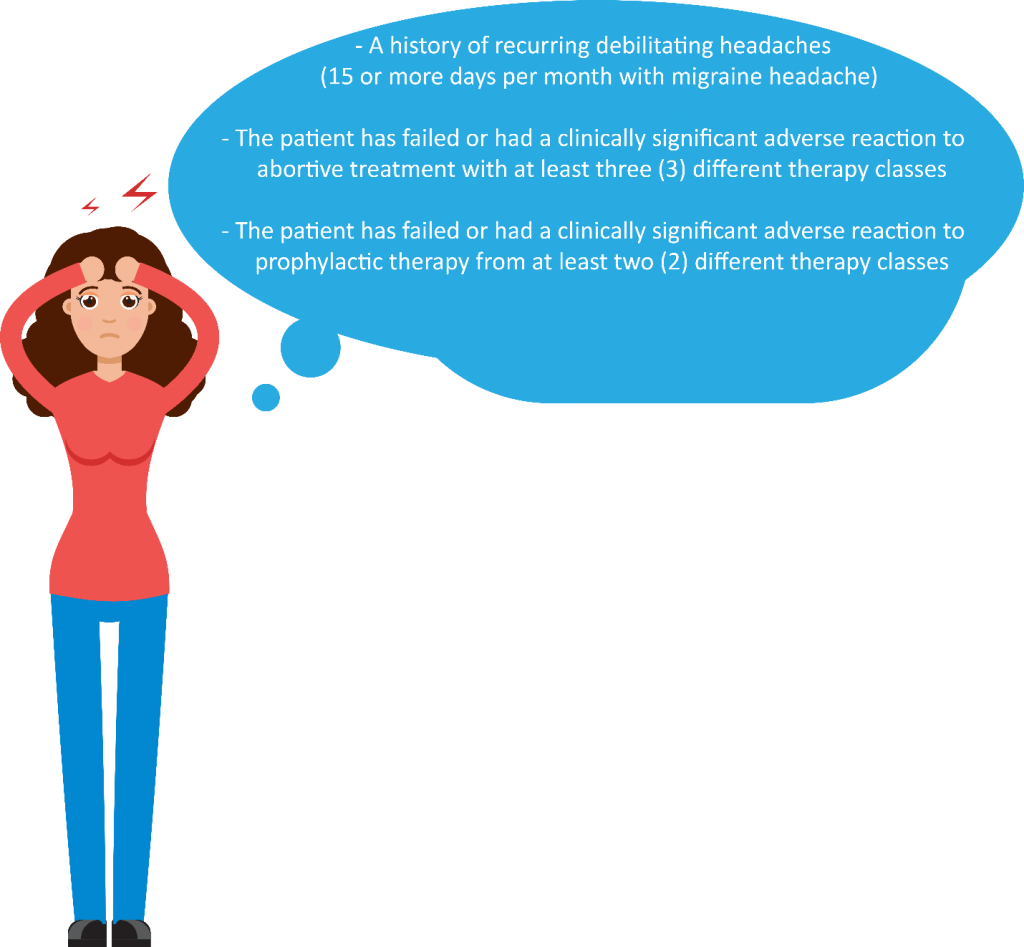
As you can see, these requirements are very specific to the treatment requiring approval.
Although the process to obtain pre-authorization may seem daunting, the prescribing physician will be a good resource for learning more about the requirements and process, as they have likely had much experience working with insurance carriers to obtain these for other patients. However, even with a good doctor by your side, there is still the chance of the treatment being denied. If this happens, you can always appeal the decision.
To get a high-level overview of the appeals process, check out our previous blog.
